Get in touch with us +44 7368 420285
Nu Medical Suppliers & Innovation Ltd - 44 Orchard Avenue Liverpool UK. L14 3NQ

Common Conditions Treated at NMSI Holistic Care
Treatment By Injury Area
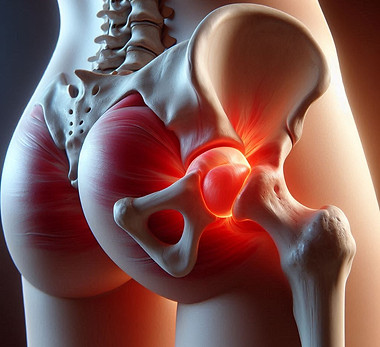
Trochanteric Bursitis / Greater Trochanteric Pain Syndrome
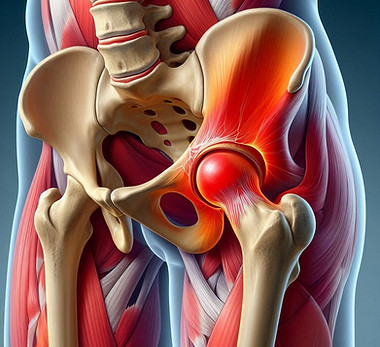
Trochanteric Bursitis (Greater Trochanteric Pain Syndrome) is a common cause of lateral hip pain, often resulting from inflammation of the bursa overlying the greater trochanter of the femur. It can be caused by repetitive stress, direct trauma, or underlying conditions like gluteal tendinopathy. Patients typically experience tenderness on the outer hip, pain with lying on the affected side, and discomfort during activities such as walking or climbing stairs.
Trigger Finger (Stenosing Tenosynovitis)

Trigger Finger (Stenosing Tenosynovitis) Trigger Finger is a condition that causes pain, stiffness, and a sensation of locking or catching when bending or straightening the finger. It occurs when inflammation narrows the space within the sheath surrounding the tendon in the affected finger. This can be the result of repetitive hand movements, gripping tools for extended periods, or underlying conditions such as diabetes or rheumatoid arthritis. Common symptoms include tenderness at the base of the finger or thumb, a popping or clicking sound during movement, and fingers getting stuck in a bent position before suddenly straightening with a snap — much like a trigger being released. We take an integrative approach to treating Trigger Finger by addressing not only the physical symptoms but also the underlying causes. Our personalized treatment plans may include manual therapy, targeted stretching and strengthening exercises, myofascial release, lifestyle and ergonomic adjustments, as well as complementary therapies such as Ayurvedic Therapies. By supporting the body’s natural healing processes and promoting balanced hand function, we aim to relieve discomfort, restore mobility, and prevent recurrence — helping you return to your daily activities with ease. Book in with us for a personalized and effective treatment plan that suites your lifestyle.
Trigger Thumb (Stenosing Tenosynovitis of the Thumb)

Trigger Thumb (Stenosing Tenosynovitis of the Thumb) Trigger Thumb is a condition where the thumb catches or locks in a bent position and may suddenly release with a snapping sensation. It occurs due to inflammation and thickening of the tendon sheath at the base of the thumb, making it difficult for the tendon to glide smoothly. This condition is often caused by repetitive thumb use, gripping motions, or underlying conditions such as diabetes or arthritis. Common symptoms include stiffness, especially in the morning, tenderness at the base of the thumb, a noticeable clicking or popping when moving the thumb, and sometimes the thumb becoming temporarily “stuck” in a bent position. At NMSI Holistic Care, we focus on uncovering the root causes and relieving symptoms through a comprehensive, personalized approach. Treatment may include gentle manual therapy, stretching and strengthening exercises for the thumb and hand, myofascial release, and ergonomic guidance. We also offer supportive therapies such as acupuncture, therapeutic ultrasound, and lifestyle modifications to reduce strain and inflammation. Our goal is to help restore smooth thumb movement, reduce pain, and support long-term hand health without dependency on invasive procedures. Book in with us for a personalized and effective treatment plan that suites your lifestyle.
Triceps Tendinopathy / Triceps Tendonitis

Triceps Tendinopathy, also known as Triceps Tendonitis, is a condition involving pain and inflammation in the tendon that connects the triceps muscle to the elbow. It often develops from repetitive strain, overuse—especially in pushing or weightlifting movements—or sudden increases in upper body activity. Microtears in the tendon can lead to stiffness, swelling, and aching in the back of the elbow, particularly during extension of the arm. People with this condition may experience pain during pressing motions, tenderness over the triceps tendon near the elbow, reduced strength, and discomfort when leaning on the elbow or performing overhead activities. At NMSI Holistic Care, we take a full-body, integrative approach to recovery. Our treatment plans are tailored to each individual and may include hands-on manual therapy, functional movement retraining, corrective exercises, postural re-education, and soft tissue techniques such as myofascial release. To further reduce inflammation and support healing, we may incorporate acupuncture, therapeutic ultrasound, or nutritional guidance. Our goal is not just to relieve pain, but to restore optimal arm function, address contributing factors, and prevent future injury — helping you return to pain-free movement with confidence. Book in with us for a personalized and effective treatment plan that suites your lifestyle.
Tennis Elbow (Lateral Epicondylitis)

Tennis Elbow, medically known as Lateral Epicondylitis, is a common condition caused by overuse or strain of the forearm muscles that attach to the outer part of the elbow. Despite its name, it affects not only athletes but also individuals who engage in repetitive gripping, lifting, or wrist extension—such as manual workers, office professionals, and those using tools or keyboards extensively. Typical symptoms include pain or burning on the outer elbow, weakened grip strength, and discomfort that worsens with repetitive use of the hand or wrist, such as lifting a kettle or shaking hands. We take a comprehensive, root-cause approach to treating Tennis Elbow. We focus on reducing pain and inflammation while restoring function through personalized care. Treatment may include manual therapy to release tension, specific exercises to strengthen and rebalance the forearm muscles, postural and movement assessments, and ergonomic guidance. We also offer complementary therapies such as acupuncture, therapeutic ultrasound, and myofascial release to support tissue healing and improve circulation. Our aim is to resolve pain, restore strength and resilience, and empower you with strategies to prevent recurrence — helping you return to daily activities with confidence and comfort. Book in with us for a personalized and effective treatment plan that suites your lifestyle.
Rotator Cuff Injury / Dysfunction
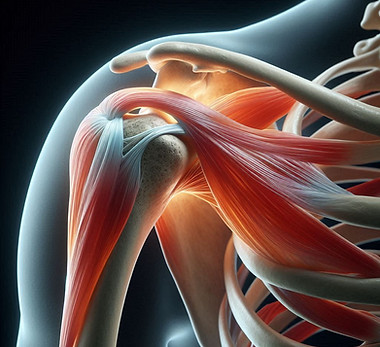
The rotator cuff is a group of four muscles and tendons that stabilize the shoulder and allow for a wide range of arm movements. Injury or dysfunction in this area can occur due to repetitive overhead activity, poor posture, trauma, or age-related wear and tear. Common conditions include rotator cuff tendinopathy, partial tears, or impingement syndrome. People with rotator cuff issues often experience shoulder pain—especially when lifting the arm, reaching behind the back, or sleeping on the affected side. Weakness, stiffness, and reduced range of motion are also common, potentially affecting daily tasks like dressing, driving, or carrying objects. At our holistic rehabilitation clinic, we approach rotator cuff injuries with a comprehensive, whole-body mindset. Our personalised treatment plans may include manual therapy, corrective and strengthening exercises, postural alignment work, and functional movement retraining. To support healing and reduce inflammation, we also offer adjunct therapies such as acupuncture, therapeutic ultrasound, and myofascial release. By addressing both the symptoms and the underlying contributing factors—such as biomechanics, muscle imbalances, or stress-related tension—we aim to restore shoulder function, reduce pain, and help you return to daily life with ease and confidence. Book in with us for a personalized and effective treatment plan that suites your lifestyle.
Rheumatoid Arthritis (RA)

Rheumatoid Arthritis is a chronic autoimmune condition where the body’s immune system mistakenly attacks the joints, causing inflammation, pain, stiffness, and swelling—most commonly in the hands, wrists, knees, and feet. Unlike osteoarthritis, which is typically related to wear and tear, RA can affect multiple joints symmetrically and may also impact overall health, energy levels, and even organs if left unmanaged. People living with RA often experience joint stiffness (especially in the morning or after rest), fatigue, reduced mobility, and flare-ups that can interfere with daily activities and quality of life. At NMSI Holistic Care, we offer an integrative approach to managing Rheumatoid Arthritis that supports both symptom relief and long-term well-being. Our personalised care plans may include gentle manual therapy, joint-friendly mobility exercises, postural correction, and strategies for energy conservation. We also provide supportive therapies such as acupuncture, myofascial release, therapeutic ultrasound, and nutritional guidance to help modulate inflammation and enhance immune balance. By working collaboratively with each individual, we aim to reduce pain, preserve joint function, and promote resilience—empowering you to navigate life with greater comfort and confidence. Book in with us for a personalized and effective treatment plan that suites your lifestyle.
Plantar Fibroma
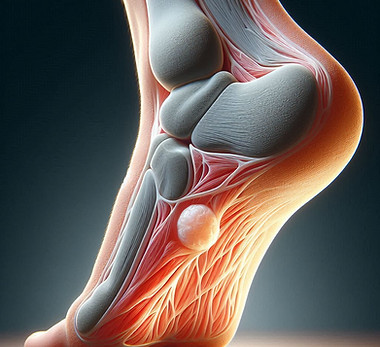
Plantar Fibroma is a benign (non-cancerous) growth or nodule that develops in the arch of the foot within the plantar fascia—the thick band of connective tissue that supports the foot’s arch. While the exact cause is not always clear, it may be associated with repetitive strain, trauma, or genetic predisposition. Over time, the fibroma can become painful, especially when walking, standing for long periods, or wearing certain footwear. Typical symptoms include a firm lump in the arch of the foot, discomfort when pressure is applied, and altered foot mechanics that may lead to further discomfort or compensatory issues in the legs, knees, or back. We take an integrative approach to managing Plantar Fibroma, aiming to reduce pain, support foot function, and improve overall mobility. Treatment may include manual therapy to reduce fascial tension, custom stretching and strengthening exercises, orthotic advice, and myofascial release techniques. Complementary therapies such as acupuncture, therapeutic ultrasound, and lifestyle or footwear modifications may also be recommended to support healing and alleviate pressure on the affected area. Our goal is to help you walk comfortably again, prevent further strain, and restore natural movement patterns through a treatment plan tailored to your individual needs. Book in with us for a personalized and effective treatment plan that suites your lifestyle.
Plantar Fasciitis
Plantar Fasciitis is one of the most common causes of heel and foot pain, resulting from inflammation or microtears in the plantar fascia—a thick band of connective tissue that runs along the bottom of the foot, connecting the heel bone to the toes. It’s often caused by repetitive stress, poor foot mechanics, improper footwear, or prolonged standing and walking on hard surfaces. Symptoms typically include sharp heel pain, especially with the first steps in the morning or after periods of rest, discomfort that worsens after activity, and tightness in the arch of the foot. At NMSI Holistic Care, we take a comprehensive, root-cause approach to treating Plantar Fasciitis. Our personalized treatment plans may include hands-on manual therapy, myofascial release, specific mobility and strengthening exercises for the feet and calves, postural retraining, and gait analysis. To further support healing and reduce inflammation, we may incorporate therapies such as acupuncture, therapeutic ultrasound, and guidance on appropriate footwear or orthotics. By addressing not just the site of pain but the underlying imbalances contributing to it, we aim to restore comfort, improve foot function, and help you return to your daily activities with greater ease and confidence. Book in with us for a personalized and effective treatment plan that suites your lifestyle.
Carpal Tunnel Syndrome

Carpal Tunnel Syndrome (CTS) is a common condition caused by compression of the median nerve as it passes through the narrow carpal tunnel in the wrist. This compression leads to symptoms such as pain, numbness, tingling, and weakness in the thumb, index, middle, and part of the ring finger. CTS often develops from repetitive wrist motions, prolonged typing, wrist positioning, or conditions like inflammation and swelling. Typical symptoms include numbness or tingling in the fingers, especially at night, weakness in grip strength, discomfort or aching in the wrist or forearm, and difficulty performing fine motor tasks such as buttoning clothes or typing. We take a personalised, root-cause approach to managing Carpal Tunnel Syndrome. Beyond treating the symptoms, we assess the entire wrist, forearm, shoulder, and neck to identify biomechanical imbalances, postural issues, or repetitive strain contributing to nerve irritation. Our treatment may include manual therapy to improve nerve mobility and reduce soft tissue restrictions, targeted exercises to strengthen the wrist and improve posture, and myofascial release to alleviate tension in the forearm muscles. We also offer supportive therapies like dry needling, therapeutic ultrasound, and ergonomic advice to modify activities and reduce strain on the wrist. Where appropriate, we may coordinate with your healthcare provider for splinting or other medical interventions to support nerve healing. Our goal is to relieve nerve pressure, restore function, reduce pain, and help you regain confidence in your daily and work activities. Book a consultation today to receive a personalised treatment plan tailored to your lifestyle and recovery goals.
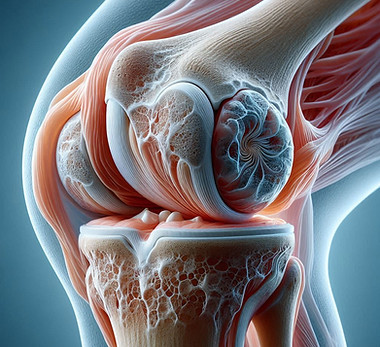
Osteoarthritis (OA)
.jpeg)
Osteoarthritis is a degenerative joint condition that occurs when the protective cartilage that cushions the ends of the bones gradually wears down over time. It is the most common form of arthritis and often affects weight-bearing joints such as the knees, hips, spine, and hands. While it’s commonly associated with ageing, other contributing factors include joint overuse, previous injury, poor biomechanics, or excess weight. Typical symptoms include joint pain and stiffness, especially after rest or activity, reduced range of motion, swelling, and sometimes a grating or clicking sensation during movement. Over time, these symptoms can impact mobility, independence, and overall quality of life. We offer a comprehensive and personalised approach to managing Osteoarthritis. Rather than focusing solely on symptom relief, we work to improve joint function, reduce inflammation, and support long-term mobility. Treatment may include gentle manual therapy, joint-specific strengthening and mobility exercises, postural and gait correction, and myofascial release. We may also incorporate supportive therapies such as acupuncture, therapeutic ultrasound, and nutritional guidance aimed at reducing systemic inflammation. Our goal is to empower you with the tools and support you need to move with greater ease, reduce discomfort, and maintain an active, fulfilling lifestyle. Book in with us for a personalized and effective treatment plan that suites your lifestyle.
Olecranon Bursitis
Olecranon Bursitis is a condition characterized by inflammation of the bursa—a small fluid-filled sac—located over the bony tip of the elbow (the olecranon). This bursa helps reduce friction between the skin and bone, but when irritated or injured, it can become swollen, painful, and tender. Causes may include repetitive pressure (such as leaning on the elbows), direct trauma, infection, or underlying inflammatory conditions like gout or rheumatoid arthritis. Common symptoms include visible swelling at the back of the elbow, discomfort when bending the arm or applying pressure, and reduced range of motion if the swelling becomes significant. We address Olecranon Bursitis through an integrative and person-centred approach. Our treatment plans aim to relieve inflammation, restore comfort, and prevent recurrence. Depending on the root cause, care may include gentle manual therapy, soft tissue techniques, postural and ergonomic advice, and exercises to reduce stress on the elbow joint. Complementary therapies such as acupuncture, therapeutic ultrasound, and anti-inflammatory lifestyle or nutritional strategies may also be recommended to support healing. Our goal is to help you regain full, pain-free function of the arm while addressing the broader movement and health patterns that contribute to lasting recovery. Book in with us for a personalized and effective treatment plan that suites your lifestyle.
Morton Neuroma

Morton’s Neuroma is a painful condition affecting the ball of the foot, most commonly between the third and fourth toes. It involves the thickening of tissue around a nerve leading to the toes, often as a result of irritation, compression, or repetitive stress. High-impact activities, tight or ill-fitting shoes, and altered foot mechanics are common contributing factors. Symptoms typically include a sharp, burning pain in the forefoot, tingling or numbness in the toes, and the sensation of walking on a small pebble or fold in a sock. Discomfort often increases with walking, running, or wearing tight shoes. At NMSI Holistic Care, we take an integrative, root-cause approach to managing Morton’s Neuroma. Our personalised treatment plans are designed to reduce nerve irritation, correct biomechanical imbalances, and promote long-term foot health. Care may include manual therapy, targeted foot and lower limb exercises, footwear advice, myofascial release, and gait retraining. We may also incorporate supportive therapies such as acupuncture, therapeutic ultrasound, and lifestyle modifications to reduce stress on the affected area. By addressing both the symptoms and underlying causes, we aim to relieve pain, restore comfort, and help you return to movement with greater confidence and ease. Book in with us for a personalized and effective treatment plan that suites your lifestyle.
Ligament Injuries

Ligaments are strong, fibrous bands of connective tissue that stabilize joints by connecting bones to one another. A ligament injury—often referred to as a sprain—occurs when these tissues are overstretched or torn, typically due to sudden impact, twisting movements, or trauma during sport, exercise, or daily activity. Commonly affected areas include the ankles, knees, wrists, and shoulders. Symptoms may include pain, swelling, bruising, joint instability, and difficulty bearing weight or moving the joint. The severity can range from mild (a stretch or micro-tear) to severe (a complete rupture), each requiring specific levels of care and rehabilitation. We take a comprehensive and tailored approach to treating ligament injuries. We focus not only on healing the injured tissue, but also on restoring joint stability, addressing imbalances, and preventing re-injury. Treatment may include hands-on manual therapy, progressive strengthening and stability exercises, movement retraining, and postural correction. To enhance tissue repair and manage inflammation, we may also use supportive therapies such as acupuncture, therapeutic ultrasound, and nutrition or lifestyle guidance. Whether you're recovering from a recent injury or dealing with long-term joint instability, our aim is to support your body’s natural healing process and help you regain strength, mobility, and confidence. Book in with us for a personalized and effective treatment plan that suites your lifestyle.
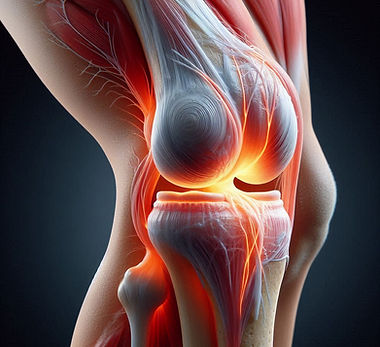
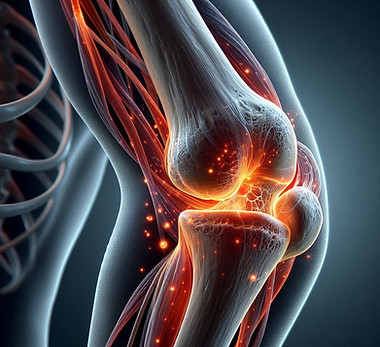
Knee Tendinitis (Patellar Tendinopathy / Jumper’s Knee)
.jpeg)
Knee Tendinitis—also commonly known as Patellar Tendinopathy or Jumper’s Knee—is an overuse injury that involves inflammation or degeneration of the tendon connecting the kneecap (patella) to the shinbone. It is often caused by repetitive stress from activities that involve jumping, running, or frequent changes in direction, and can also result from poor biomechanics, muscular imbalances, or tightness in surrounding tissues. Symptoms typically include pain and tenderness at the front of the knee, just below the kneecap, which may worsen during activity or after prolonged sitting. You may also experience stiffness, swelling, or a sensation of weakness during movement. At our holistic rehabilitation clinic, we take a personalised, root-cause approach to managing Knee Tendinitis. Rather than only addressing the pain, we assess the entire kinetic chain to uncover underlying factors contributing to the tendon irritation. Treatment may include hands-on manual therapy, targeted strengthening and mobility exercises, myofascial release, and movement retraining. We also offer supportive therapies such as acupuncture, therapeutic ultrasound, and ergonomic or activity-specific advice to reduce strain on the knee. Our goal is to restore strength and resilience to the tendon, promote healing, and help you return to your daily and athletic activities with confidence and long-term stability. Book in with us for a personalized and effective treatment plan that suites your lifestyle.
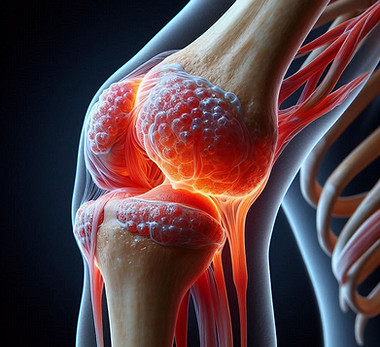
Knee Joint Arthritis
Knee Joint Arthritis is a degenerative condition that involves the breakdown of cartilage in the knee joint, leading to pain, stiffness, and reduced mobility. The most common form is Osteoarthritis, though Rheumatoid Arthritis and other inflammatory types can also affect the knee. Contributing factors may include age-related wear and tear, previous injury, biomechanical imbalances, excess weight, or chronic inflammation. Common symptoms include pain with movement or after prolonged inactivity, swelling, stiffness (especially in the morning or after rest), a grinding or clicking sensation in the joint, and difficulty with activities like walking, climbing stairs, or kneeling. We take an integrative, whole-body approach to managing Knee Joint Arthritis. Our personalised care plans are designed to reduce pain, improve joint function, and support long-term mobility. Treatment may include joint-specific strengthening and mobility exercises, hands-on manual therapy, postural correction, and gait retraining. We also offer supportive therapies such as acupuncture, myofascial release, therapeutic ultrasound, and nutritional guidance to reduce inflammation and promote tissue health. Our goal is to empower you with the tools, strategies, and support needed to move with greater comfort and ease—while addressing the underlying causes to prevent further degeneration. Book in with us for a personalized and effective treatment plan that suites your lifestyle.
Knee Bursitis
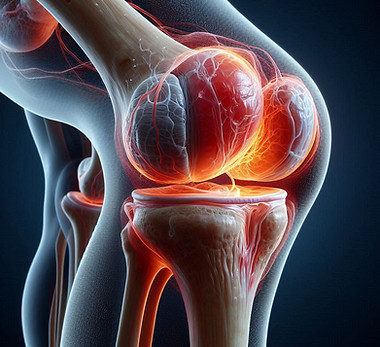
Knee Bursitis is a condition that involves inflammation of one or more bursae around the knee joint. Bursae are small, fluid-filled sacs that act as cushions between bones, tendons, and muscles, helping to reduce friction during movement. When these sacs become irritated—often due to overuse, prolonged kneeling, trauma, or underlying inflammatory conditions—they can swell and become painful. Common types include prepatellar bursitis (in front of the kneecap), infrapatellar bursitis (below the kneecap), and pes anserine bursitis (on the inner side of the knee). Symptoms typically include localized swelling, tenderness, warmth, and pain that worsens with movement or pressure. In more severe cases, range of motion may be limited, and the area may feel stiff or appear red. At our holistic rehabilitation clinic, we take a whole-person, root-cause approach to treating Knee Bursitis. Rather than just reducing the inflammation, we assess contributing factors such as joint alignment, muscular imbalances, biomechanics, and repetitive strain patterns that may be aggravating the bursae. Our treatment plan may include gentle manual therapy to relieve pressure around the inflamed bursa, targeted strengthening and mobility exercises to support surrounding structures, myofascial release, and movement retraining. Supportive therapies such as therapeutic ultrasound, dry needling, acupuncture, or ultrasound-guided injections (e.g., corticosteroids or PRP) may also be recommended when appropriate. We provide ergonomic advice and activity modifications to help prevent recurrence and promote long-term knee health. Our aim is to relieve discomfort, restore optimal knee function, and help you return to your activities with lasting confidence and ease. Book an appointment today for a personalised treatment plan tailored to your lifestyle and recovery goals.
Ischial bursitis
Ischial Bursitis—also known as Ischiogluteal Bursitis or "weaver’s bottom"—is a condition caused by inflammation of the bursa located between the ischial tuberosity (the sitting bone) and the overlying gluteal muscles. This bursa helps cushion and reduce friction in the lower pelvis, especially during sitting and movement involving the hips. When it becomes irritated from prolonged sitting, direct trauma, or repetitive stress, inflammation and pain can develop. Common symptoms include a deep, aching pain in the buttock region, especially while sitting, climbing stairs, or stretching the hamstrings. The pain may radiate down the back of the thigh, often mimicking sciatica. In some cases, swelling, tenderness, or stiffness may also be felt around the sitting bone. At our holistic rehabilitation clinic, we take a personalised, root-cause approach to managing Ischial Bursitis. We go beyond just treating the inflamed bursa by assessing the entire lumbopelvic region, including postural imbalances, muscle tension, and movement habits that may be contributing to chronic irritation. Treatment may involve hands-on manual therapy to reduce muscle tightness and pressure around the bursa, specific strengthening and mobility exercises to stabilise the pelvis and hips, myofascial release, and movement re-education. Supportive therapies such as dry needling, acupuncture, therapeutic ultrasound, or guided injections (e.g., corticosteroid or PRP) may be incorporated as needed. We also provide advice on sitting ergonomics, activity modification, and stretching routines to help manage symptoms and prevent recurrence. Our goal is to relieve pain, restore functional mobility, and support your return to daily activities—pain-free and with improved comfort. Schedule a consultation with us to receive a personalised and effective treatment plan tailored to your unique needs and lifestyle.
Hip pain Arthritis

Most commonly known as osteoarthritis—is a degenerative joint condition that affects the cartilage within the hip joint. As the protective cartilage wears down over time due to age, repetitive strain, injury, or inflammation, the bones may rub against each other, leading to pain, stiffness, and reduced mobility. Other forms such as rheumatoid arthritis, psoriatic arthritis, or post-traumatic arthritis can also contribute to hip joint deterioration. Typical symptoms include deep aching pain in the groin, outer thigh, or buttock, which may worsen with activity, prolonged standing, or after periods of rest. You may notice reduced range of motion, stiffness (especially in the morning), difficulty walking, limping, and discomfort while bending or climbing stairs. We take a whole-body, root-cause approach to managing Hip Arthritis. Rather than focusing solely on relieving joint pain, we assess the entire kinetic chain—including your spine, pelvis, and lower limbs—to uncover biomechanical imbalances, muscular weakness, and movement patterns that may be overloading the hip joint. Our treatment approach may include gentle manual therapy to improve joint mobility, targeted exercises to strengthen supporting muscles, myofascial release to reduce tension, and functional movement retraining. Complementary therapies such as acupuncture, dry needling, therapeutic ultrasound, or ultrasound-guided injections (e.g., hyaluronic acid, corticosteroids, or PRP) may also be offered when appropriate. We provide personalised advice on joint-protective strategies, daily movement modifications, and weight management support if needed. Our goal is to relieve pain, restore hip function, and empower you with the tools and strategies to move confidently and comfortably through daily life. Book your consultation today and take the first step toward long-term relief and functional freedom.
Gouty Arthritis

Gouty Arthritis, commonly referred to as Gout, is a form of inflammatory arthritis caused by a buildup of uric acid crystals in the joints. This buildup can lead to sudden and intense episodes of joint pain, swelling, redness, and heat—most often affecting the big toe, but it can also involve the ankles, knees, wrists, fingers, and elbows. Gout attacks often occur at night and may be triggered by dietary factors, dehydration, certain medications, or underlying metabolic imbalances. Over time, if not properly managed, recurrent gout attacks can lead to chronic joint damage, reduced mobility, and the formation of tophi—hard lumps of uric acid crystals under the skin. Common symptoms include severe, sharp joint pain (often in a single joint), warmth and redness over the joint, swelling, and tenderness that can make even light contact unbearable. Some people may also experience fever or a general sense of being unwell during a flare-up. We approach Gouty Arthritis with a comprehensive, root-cause strategy that goes beyond simply treating flare-ups. We aim to understand the underlying contributors such as poor metabolic function, dietary imbalances, kidney health, and lifestyle habits that may be raising uric acid levels and straining the joints. Treatment may involve gentle manual therapy during non-acute phases, mobility and strengthening exercises to support joint health, anti-inflammatory modalities like acupuncture or therapeutic ultrasound, and supportive dietary and lifestyle guidance. Where appropriate, we may also collaborate with your healthcare provider to integrate lab testing, medication support, or referrals for advanced care. Our focus is on reducing inflammation, preventing future attacks, protecting joint integrity, and helping you live comfortably with confidence and control over your symptoms. Book an appointment with us today to receive a personalised care plan that supports your whole-body health and long-term wellness.
Golfers elbow
Golfer’s Elbow—medically known as Medial Epicondylitis—is an overuse injury that causes pain and inflammation in the tendons that attach to the inner side of the elbow. Despite the name, this condition is not limited to golfers; it can affect anyone who performs repetitive wrist flexion or gripping activities, such as lifting, typing, throwing, or using tools. The condition typically develops gradually and is caused by repetitive stress on the forearm muscles that control wrist and finger movements. Poor technique, muscle imbalances, and inadequate recovery from repetitive strain often contribute to the development of Golfer’s Elbow. Common symptoms include aching or burning pain on the inside of the elbow, stiffness, tenderness to touch, weakness in the wrist or hand, and pain that worsens with certain activities like gripping, lifting, or twisting motions. We take a personalised, root-cause approach to managing Golfer’s Elbow. Rather than just treating the symptoms, we assess the entire upper limb, shoulder, neck, and posture to identify contributing factors such as poor biomechanics, muscle imbalances, or improper movement patterns. Treatment may include hands-on manual therapy to release tension and improve soft tissue health, targeted exercises to strengthen and stretch the forearm muscles, myofascial release, and movement retraining. We may also incorporate supportive therapies such as dry needling, therapeutic ultrasound, acupuncture, or ergonomic guidance to reduce ongoing strain on the elbow. Our goal is to reduce pain and inflammation, restore strength and flexibility, and help you return to your daily or athletic activities with long-term resilience and confidence.
Ganglion Cyst

A Ganglion Cyst is a non-cancerous, fluid-filled lump that commonly develops along the joints or tendons of the wrist, hand, ankle, or foot. These cysts are usually round or oval, and while they may vary in size, they are often noticeable just under the skin. Ganglion cysts are filled with a thick, jelly-like fluid and may fluctuate in size or even disappear temporarily. Although the exact cause is not always known, they are often associated with joint or tendon irritation, repetitive strain, or injury. They are most commonly seen in people who perform repetitive wrist or hand movements, such as athletes, typists, or manual workers. Symptoms may include a visible lump, discomfort or pain (especially with joint movement or pressure on the cyst), stiffness, and sometimes weakness in the affected area. In some cases, the cyst may press on nearby nerves, leading to tingling or numbness. We take a whole-person, functional approach to managing Ganglion Cysts. While some cysts may resolve on their own, persistent or painful cases require a more strategic plan to address both the symptoms and any underlying mechanical stress contributing to the condition. Treatment may involve manual therapy to relieve tension and improve mobility in the surrounding joints, myofascial release to reduce strain on tissues, and targeted exercises to support joint stability. We may use therapeutic ultrasound, acupuncture, or dry needling to help improve circulation and tissue healing. If appropriate, ultrasound-guided aspiration or referral for further medical management can be coordinated. Our focus is not only to manage the cyst itself but also to correct any biomechanical or functional issues that may be contributing to its formation or persistence—helping you reduce recurrence and regain full, pain-free movement. Book a consultation with us today to receive a personalised care plan tailored to your needs and lifestyle.
Elbow Joint Rheumatoid Arthritis

Elbow Joint Rheumatoid Arthritis is an autoimmune condition that causes chronic inflammation of the synovial lining of the elbow joint. Unlike osteoarthritis, which results from wear and tear, Rheumatoid Arthritis (RA) is a systemic disease where the body’s immune system mistakenly attacks healthy joint tissue, leading to pain, swelling, stiffness, and progressive joint damage. The elbow is one of the joints commonly affected in people with RA, and involvement is often symmetrical, meaning both elbows may be affected. Over time, inflammation can lead to joint instability, reduced range of motion, and deformity if left unmanaged. Symptoms include persistent pain, swelling, warmth, and stiffness around the elbow joint—especially in the morning or after periods of inactivity. Many people also experience fatigue, muscle weakness, and difficulty performing tasks that involve pushing, lifting, or gripping. Our integrated, whole-body approach to managing Rheumatoid Arthritis of the elbow. In addition to supporting symptom relief, we focus on improving joint function, preventing deformity, and addressing the root causes of inflammation and dysfunction in the body. Our treatment plan may include gentle manual therapy to maintain joint mobility, tailored strengthening and mobility exercises to support the surrounding muscles, and myofascial release to reduce tissue tension. We also offer supportive therapies such as acupuncture, dry needling, and therapeutic ultrasound to manage pain and inflammation. Where appropriate, ultrasound-guided injections (e.g., corticosteroids) may be recommended in collaboration with your healthcare provider. We complement our physical treatments with lifestyle and ergonomic guidance, helping you modify daily activities, reduce joint strain, and manage flares more effectively. Our team works with you to create a sustainable plan that supports long-term joint health and whole-person wellness. Book a consultation today to start a personalised and compassionate care plan for managing Rheumatoid Arthritis of the elbow.
Frozen shoulder

Frozen Shoulder, also known as Adhesive Capsulitis, is a condition characterized by stiffness, pain, and progressive loss of movement in the shoulder joint. It occurs when the capsule of connective tissue surrounding the shoulder becomes inflamed, thickened, and tight, restricting joint mobility. Frozen Shoulder often develops gradually and can severely impact daily activities and quality of life. This condition typically progresses through three phases: Freezing phase – Increasing pain and gradual loss of shoulder movement Frozen phase – Stiffness becomes the dominant symptom; pain may reduce Thawing phase – Gradual return of mobility over time Common causes include shoulder immobility following injury or surgery, certain medical conditions (e.g., diabetes, thyroid disorders), or it may occur idiopathically (without a clear cause). Symptoms include deep, aching shoulder pain, stiffness, restricted range of motion (especially with reaching or rotating), and discomfort during sleep or overhead activities. We take a comprehensive, root-cause approach to managing Frozen Shoulder. Rather than simply focusing on relieving pain, we assess the entire shoulder girdle, spine, posture, and movement patterns to uncover underlying factors contributing to the restriction. Treatment may include gentle manual therapy to improve joint mobility, myofascial release to address tight surrounding tissues, and progressive, pain-free mobility and strengthening exercises to restore function. We also offer supportive therapies such as dry needling, acupuncture, therapeutic ultrasound, and hydrodilatation injections (under ultrasound guidance) to reduce capsular tightness and inflammation when appropriate. Our goal is to reduce pain, restore range of motion, and help you confidently return to your daily activities with improved shoulder function and comfort. Book a consultation today to receive a personalised treatment plan tailored to your stage of recovery and lifestyle needs.
Elbow Joint Osteoarthritis

Elbow Joint Osteoarthritis is a degenerative condition that results from the gradual wear and tear of the cartilage that cushions the elbow joint. As this protective cartilage breaks down over time, the bones within the joint begin to rub against each other, leading to pain, stiffness, swelling, and reduced range of motion. Though less common than osteoarthritis in the knees or hips, elbow osteoarthritis can significantly affect daily activities involving arm movement and load-bearing. This condition may develop due to age-related degeneration, previous elbow injuries (such as fractures or dislocations), repetitive strain from manual labor or sports, or long-term joint stress. Over time, bony growths called osteophytes may form, further restricting movement and causing discomfort. Typical symptoms include aching pain in the elbow, stiffness (especially in the morning or after inactivity), grinding or clicking sensations, reduced flexibility, and difficulty with tasks like lifting, pushing, or fully extending the arm. Our whole-person, root-cause approach to managing Elbow Osteoarthritis. Rather than focusing only on the site of pain, we assess your entire upper limb mechanics, posture, shoulder and wrist function, and lifestyle habits to understand the full picture and reduce strain on the joint. Our treatment may include gentle manual therapy to mobilise the elbow, myofascial release to reduce tension in surrounding muscles, and targeted exercises to improve strength, flexibility, and joint stability. Supportive therapies such as therapeutic ultrasound, acupuncture, dry needling, or ultrasound-guided injections (such as corticosteroids or hyaluronic acid) may be incorporated as needed to reduce inflammation and pain. We also provide ergonomic advice, activity modification strategies, and home-care guidance to support joint health and prevent flare-ups. Our goal is to enhance elbow function, minimise discomfort, and help you maintain independence in your work, hobbies, and daily routine. Book a consultation today and begin your personalised journey toward better elbow health and long-term joint resilience.
Distal Bicep Tendonitis

Distal Bicep Tendonitis is an overuse injury that affects the tendon connecting the biceps muscle to the radius bone near the elbow. This tendon plays a key role in bending the elbow and rotating the forearm. Repetitive stress, sudden heavy lifting, or poor biomechanics can cause irritation, inflammation, and microscopic tears in the tendon, leading to pain and discomfort. Symptoms typically include pain and tenderness at the front of the elbow, swelling, and a sensation of weakness when bending the arm or rotating the forearm (such as turning a doorknob or using a screwdriver). Pain may worsen with activity, especially lifting or gripping, and may be accompanied by stiffness or discomfort during rest. We adopt a personalised, root-cause approach to treating Distal Bicep Tendonitis. Instead of focusing solely on symptom relief, we assess the entire arm, shoulder, and movement patterns to identify and address underlying factors such as muscle imbalances, poor technique, or joint restrictions that contribute to tendon overload. Our treatment plan may include manual therapy to reduce tendon tension and improve mobility, targeted strengthening and flexibility exercises to restore tendon resilience, and myofascial release to alleviate tightness in surrounding muscles. Supportive therapies like dry needling, therapeutic ultrasound, and acupuncture may be offered to reduce inflammation and promote healing. In some cases, ultrasound-guided injections can also be considered to assist recovery. Our goal is to relieve pain, restore strength and function, and help you return to your daily activities or sports with confidence and long-term tendon health. Book your consultation today for a tailored treatment plan that fits your lifestyle and recovery goals.
De Quervain’s Tenosynovitis

De Quervain’s Tenosynovitis is a painful condition affecting the tendons on the thumb side of the wrist. It occurs when the tendons controlling thumb movement become irritated or inflamed as they pass through a narrow tunnel near the wrist, leading to pain and swelling. This condition is often caused by repetitive hand or wrist movements, overuse, or strain from gripping, lifting, or twisting motions. Common symptoms include sharp pain at the base of the thumb and wrist, tenderness, swelling, and difficulty gripping or pinching. Movements such as turning a key, holding a cup, or texting can aggravate the discomfort. Some people also experience a catching or snapping sensation when moving the thumb. We take a personalised, root-cause approach to managing De Quervain’s Tenosynovitis. Beyond simply addressing the inflammation, we assess the entire hand, wrist, forearm, and posture to identify movement patterns, muscle imbalances, or ergonomic factors that may be contributing to ongoing tendon irritation. Treatment may include gentle manual therapy to reduce tendon and soft tissue restrictions, myofascial release, and targeted exercises to improve strength, flexibility, and coordination of the wrist and thumb. We also offer supportive therapies such as dry needling, therapeutic ultrasound, and acupuncture to promote healing and reduce pain. Where appropriate, we can assist with ergonomic advice and activity modifications to reduce strain during daily tasks. Our goal is to relieve pain, restore smooth tendon movement, and help you regain full function and comfort in your wrist and hand. Book a consultation today for a customised treatment plan designed to support your recovery and return to pain-free activity.
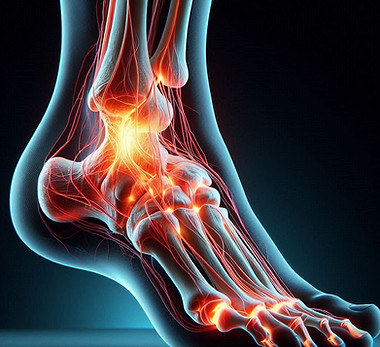
Achilles Tendinitis
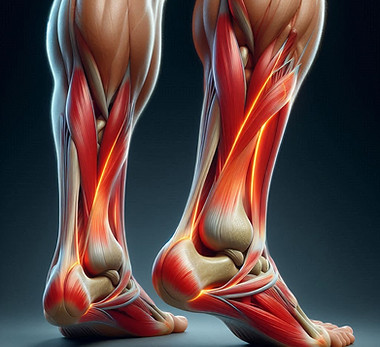
Achilles Tendinitis is an overuse injury characterized by inflammation or degeneration of the Achilles tendon, the strong band of tissue that connects the calf muscles to the heel bone. It commonly occurs due to repetitive stress from activities such as running, jumping, or sudden increases in physical activity, and can also be influenced by poor footwear, tight calf muscles, or biomechanical imbalances. Symptoms usually include pain and stiffness along the back of the heel and lower calf, which may worsen with activity or after periods of rest. You might notice swelling, tenderness to touch, and a sensation of tightness in the tendon, especially in the morning or after exercise. We take a personalised, root-cause approach to managing Achilles Tendinitis. We don’t just focus on symptom relief; we assess your entire lower limb biomechanics, calf muscle flexibility, foot posture, and movement patterns to identify underlying factors contributing to tendon overload. Our treatment plan may include hands-on manual therapy to improve tendon and muscle flexibility, targeted strengthening exercises to build resilience in the calf and surrounding muscles, and myofascial release to reduce tension. We also offer supportive therapies such as dry needling, therapeutic ultrasound, and ultrasound-guided injections when appropriate, to reduce inflammation and promote healing. Additionally, we provide guidance on footwear, activity modification, and gradual return-to-sport programs to prevent recurrence and support long-term tendon health. Our goal is to relieve pain, restore tendon strength and flexibility, and help you return confidently to your daily activities or athletic pursuits. Book your consultation today for a personalised treatment plan designed to get you back on your feet stronger and pain-free.